Michael S. Shafer, Ph.D.
Pacific Southwest Addiction Technology Transfer Center
Arizona State University
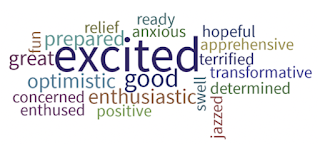
February 4-6, 2020, 39 behavioral health professionals representing 13 agencies throughout HHS Region 9 gathered in Oakland, California for three days to participate in the PSATTC’s Organizational Process Improvement Initiative (OPII) Change Facilitator Academy, launching a 10-month, long-term intensive technical assistance program. Each agency’s group of newly trained facilitators returned home with a plan to brief their Executive Sponsor (who had previously provided a letter of commitment for staff to attend) and hold an organizational change team kick off meeting within 30-45 days. Schedules were coordinated to ensure that I could travel to and attend each of these meetings; no small feat considering sites were located in two states (CA & AZ) and two Pacific Jurisdictions (RMI & CNMI) half a world away. This wordle, captured at the conclusion of the 3-day Academy, denotes the spirit and emotion of the participants.
Pacific Southwest Addiction Technology Transfer Center
Arizona State University
February 4-6, 2020, 39 behavioral health professionals representing 13 agencies throughout HHS Region 9 gathered in Oakland, California for three days to participate in the PSATTC’s Organizational Process Improvement Initiative (OPII) Change Facilitator Academy, launching a 10-month, long-term intensive technical assistance program. Each agency’s group of newly trained facilitators returned home with a plan to brief their Executive Sponsor (who had previously provided a letter of commitment for staff to attend) and hold an organizational change team kick off meeting within 30-45 days. Schedules were coordinated to ensure that I could travel to and attend each of these meetings; no small feat considering sites were located in two states (CA & AZ) and two Pacific Jurisdictions (RMI & CNMI) half a world away. This wordle, captured at the conclusion of the 3-day Academy, denotes the spirit and emotion of the participants.
These are agencies that were ready for change and innovation; they had applied to the PSATTC OPII program to enhance their ability to do so. Selected agencies were required to survey their staff using the TCU Organizational Readiness to Change Assessment. Academy participants had to view three hours of asynchronous video modules before arriving in Oakland. CEOs had to provide a letter of commitment with specific deliverables and action items associated with the OPII model.
And then COVID-19 happened. Site visits were cancelled, kick off meetings were put on hold and change teams suspended, as agencies responded with immediate crisis management actions to protect staff and patients and begin to reimagine service engagement with clients in a physically-distant manner. One agency executive director approved $80,000 in expenditures related to ramping her agency’s telehealth capacity in the two weeks following implementation of her state’s stay at home order. In late March and early April, however, the most important thing these agencies had to focus on changing and innovating was protecting their staff and patient’s safety.
In the four months since the onset of the COVID-19 pandemic, six of the 13 teams have resumed meeting regularly, virtually, and advancing in the 4-phased OPII model. Two of the agencies withdrew their participation, while one agency postponed their change team launch until July. Our ATTC team pivoted our TA procedures. We launched a series of group and individual agency email and zoom meeting communications encouraging agencies to consider altering their improvement change goal to address agency-pressing COVID related issues (such as telehealth adoption). In lieu planned site visits, I began holding Zoom check-ins with each agency every 4-6 weeks. Using Zoom’s recording and transcription capacities has proven a great innovation for documentation and evaluation purposes! We launched a monthly 1-hour Community of Practice (CoP) Zoom session to introduce virtual facilitation tools and skills (such as Zoom and Mural; this portion of the CoP is called the “spark session”) to support facilitators’ virtual team facilitation skill development. These virtual CoP sessions also afford an opportunity for agencies to check-in on their team progress in the OPII change model, while sharing facilitation successes and struggles. These communications are providing insights into the organizational resilience of these agencies in the face of massive short- and yet-to-be-defined long-term changes, and the impact of an ATTC-mediated technical assistance model on strengthening their capacity for technology transfer and innovation.
And then COVID-19 happened. Site visits were cancelled, kick off meetings were put on hold and change teams suspended, as agencies responded with immediate crisis management actions to protect staff and patients and begin to reimagine service engagement with clients in a physically-distant manner. One agency executive director approved $80,000 in expenditures related to ramping her agency’s telehealth capacity in the two weeks following implementation of her state’s stay at home order. In late March and early April, however, the most important thing these agencies had to focus on changing and innovating was protecting their staff and patient’s safety.
In the four months since the onset of the COVID-19 pandemic, six of the 13 teams have resumed meeting regularly, virtually, and advancing in the 4-phased OPII model. Two of the agencies withdrew their participation, while one agency postponed their change team launch until July. Our ATTC team pivoted our TA procedures. We launched a series of group and individual agency email and zoom meeting communications encouraging agencies to consider altering their improvement change goal to address agency-pressing COVID related issues (such as telehealth adoption). In lieu planned site visits, I began holding Zoom check-ins with each agency every 4-6 weeks. Using Zoom’s recording and transcription capacities has proven a great innovation for documentation and evaluation purposes! We launched a monthly 1-hour Community of Practice (CoP) Zoom session to introduce virtual facilitation tools and skills (such as Zoom and Mural; this portion of the CoP is called the “spark session”) to support facilitators’ virtual team facilitation skill development. These virtual CoP sessions also afford an opportunity for agencies to check-in on their team progress in the OPII change model, while sharing facilitation successes and struggles. These communications are providing insights into the organizational resilience of these agencies in the face of massive short- and yet-to-be-defined long-term changes, and the impact of an ATTC-mediated technical assistance model on strengthening their capacity for technology transfer and innovation.