Maxine Henry, MSW, MBACo-DirectorNational Hispanic and Latino ATTC
Ethnic and racial inequality has been present in our landscape for generations, yet the COVID 19 pandemic seems to have put a spotlight on the disparities felt by people of color and other minority groups. In a time where the entire world is experiencing overwhelming stress brought on by a virus that has changed our everyday lives, the National Hispanic and Latino ATTC decided to bring together powerful voices to spark conversation and activate positive change in our communities across the nation.
September is a busy month for many in the behavioral health field, as we celebrate National Recovery and Suicide Prevention Month our calendars and social media fill up with important events and inspiring messages of hope, healing and transformation. In many ways it has been a bright spot in the pandemic.
For Latinx community members September also kicks off Hispanic Heritage Month (September 15-October 15), providing us with additional opportunities to commemorate and celebrate our diverse communities. The 2020 theme for Hispanic Heritage Month is “Hispanics: Be Proud of Your Past and Embrace the Future”. In honor of this year’s theme our team decided to host a 4-part Virtual Learning Series titled “The Intersection of Acculturation, Assimilation, and Substance Use Disorder in Latinx Communities: Risk and Resiliency Factors”.
Different from a webinar format, this virtual learning community consists of a returning panel of four subject matter experts who are well respected in the areas of focus: Hector Adames, Psy.D.; Lorraine Moya Salas, PhD; Anna Nelson, LCSW; and Mr. Javier Alegre. The experts spend a short time providing an insight into the research and theories covered in our sub-topics and then have open dialogue with the same small audience of professionals, paraprofessionals, peers, students and leaders from across the U.S. This event is focused on providing a safe space for key stakeholders to gather to discuss the topics of race, disparities and strengths in the Latinx communities they come from and/or serve in the behavioral health space. The goal was to secure engagement in order for the participants to return to their communities and begin to manifest positive change.
Throughout all of our four sub-topics one theme that is consistent is radical healing as a key component to not only coping with racial and ethnic inequities and long-standing collective trauma that is the exacerbated by the pandemic, but to thrive despite the disparities that our communities have felt and, in some instances, contributed to. On its surface radical healing might sound far-fetched or hard to obtain, but once you take a closer look it is a natural strength of many communities. It is based in fundamental tenants often found in the deeply rooted Latinx culture. “Advancing beyond individual-level approaches to coping with racial trauma, we call for a new multisystemic psychological framework of radical healing for People of Color and Indigenous individuals. Radical healing involves critical consciousness, radical hope, strength and resistance, cultural authenticity, self-knowledge and collectivism. (French, Lewis, Mosley, Adames, Chavez-Dueñas, Chen, & Neville, 2019).”
Under this premise we can look back on what our ancestors have taught us, that in times of need we employ
familismo, our larger family unit consisting of relatives, friends and community. To heal, recover and thrive from trauma and/or substance use disorders we look to traditional healing, connection and collectivism to take care of ourselves and others. When we face inequities, we rely on our resilience taught to us by our ancestors and family, stand in resistance to racism, and work together to push our families into the future.
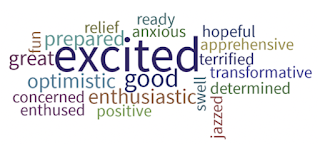
Our goal with this event is not only to unpack issues of historical trauma, racism and intersectionality but also to highlight the strength, resiliency and power of our diverse communities. Furthermore, we aspire to use this dialogue as the catalyst for community and systemic change to heal and push forward into a brighter, healthier, more equitable landscape.
REFERENCE:
French, B. H., Lewis, J. A., Mosley, D. V., Adames, H. Y., Chavez-Dueñas, N. Y., Chen, G. A.,
& Neville, H. A. (2020). Toward a Psychological Framework of Radical Healing in Communities of Color. The Counseling Psychologist, 48(1), 14-46.
https://doi.org/10.1177/0011000019843506.